Diverticulitis treatments, diagnosis and symptoms
Diverticulitis in Children and Adolescents: A Comprehensive Guide
Introduction
Diverticulitis is a gastrointestinal condition commonly associated with adults, particularly those over the age of 40. However, while it is relatively rare, it can also affect children and adolescents. In this comprehensive guide, we will delve into the diagnosis, symptoms, and treatments of diverticulitis specifically in pediatric patients. By providing an in-depth understanding of this condition, we aim to support healthcare professionals in recognizing and managing diverticulitis in children and adolescents effectively.
I. Understanding Diverticulitis in Pediatric Patients
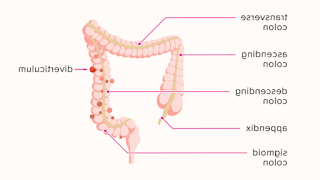
- Definition and Causes
Diverticulitis is characterized by inflamed or infected pouches, called diverticula, that form along the wall of the colon. In children and adolescents, this condition is considered secondary, meaning it arises as a result of an underlying condition or predisposing factor. Common causes of diverticulitis in pediatric patients include:
- Structural abnormalities in the colon
- Chronic constipation or irregular bowel movements
- Inflammatory bowel disease (IBD)
- Connective tissue disorders
- Familial predisposition
- Trauma or injury to the colon
- Symptoms and Diagnosis
Diagnosing diverticulitis in children and adolescents can be challenging, as the symptoms may overlap with other gastrointestinal conditions. Common symptoms include:
- Abdominal pain and tenderness, often localized in the lower left side
- Changes in bowel habits, such as diarrhea or constipation
- Rectal bleeding or blood in the stool
- Fever and general malaise
- Nausea and vomiting
- Loss of appetite and weight loss
To diagnose diverticulitis, healthcare professionals employ a combination of physical examination, medical history review, and diagnostic tests, including:
- Abdominal ultrasound
- Computed tomography (CT) scan
- Colonoscopy (rarely performed in pediatric patients)
II. Treatment Approaches for Pediatric Diverticulitis
- Non-surgical Management
The initial treatment of diverticulitis in pediatric patients typically involves non-surgical approaches. These may include:
- Antibiotics: Prescribed to manage infection and reduce inflammation.
- Bowel rest: Temporary dietary modifications, including a clear liquid or low-fiber diet, to allow the colon to heal.
- Pain management: Over-the-counter or prescription pain relievers to alleviate abdominal pain.
- Probiotics: May be recommended to restore a healthy balance of gut bacteria.
- Surgical Intervention
In some cases, pediatric diverticulitis may require surgical intervention. Surgery is usually reserved for patients who do not respond to conservative treatments or those with severe complications, such as abscesses, perforation, or fistulas. Surgical options include:
- Bowel resection: Removal of the affected portion of the colon, followed by reconnection of the healthy segments.
- Colostomy: A surgical procedure where an opening (stoma) is created on the abdomen to allow waste to pass into a bag outside the body. This may be temporary or permanent, depending on the patient's condition.
III. Long-Term Management and Prevention
- Lifestyle Modifications
To manage and prevent recurrent diverticulitis episodes in pediatric patients, certain lifestyle modifications can be beneficial. These may include:
- High-fiber diet: Encouraging the consumption of fruits, vegetables, whole grains, and legumes to promote regular bowel movements and prevent constipation.
- Hydration: Ensuring an adequate intake of fluids to maintain proper bowel function.
- Regular exercise: Physical activity helps maintain bowel regularity and overall well-being.
- Stress management: Teaching stress reduction techniques can minimize the impact of stress on the digestive system.
- Medications
In some cases, healthcare professionals may prescribe medications to manage symptoms and prevent flare-ups. Medications commonly used include:
- Fiber supplements: Recommended to ensure an adequate fiber intake.
- Laxatives: May be prescribed to alleviate constipation and promote regular bowel movements.
- Anti-inflammatory drugs: Used in patients with underlying inflammatory conditions, such as IBD.
IV. Conclusion
While diverticulitis is more commonly associated with adults, it can affect children and adolescents as well. Recognizing the symptoms, obtaining an accurate diagnosis, and implementing appropriate treatment strategies are crucial in managing pediatric diverticulitis effectively. By considering the underlying causes, employing non-surgical and surgical interventions when necessary, and implementing long-term management and prevention measures, healthcare professionals can provide optimal care for young patients with this condition. Continued research and clinical experience are essential to further understand the unique aspects of diverticulitis in pediatric populations and refine treatment approaches accordingly.
Post a Comment